Keratoconus Treatments: Understanding Your Options and Finding Relief
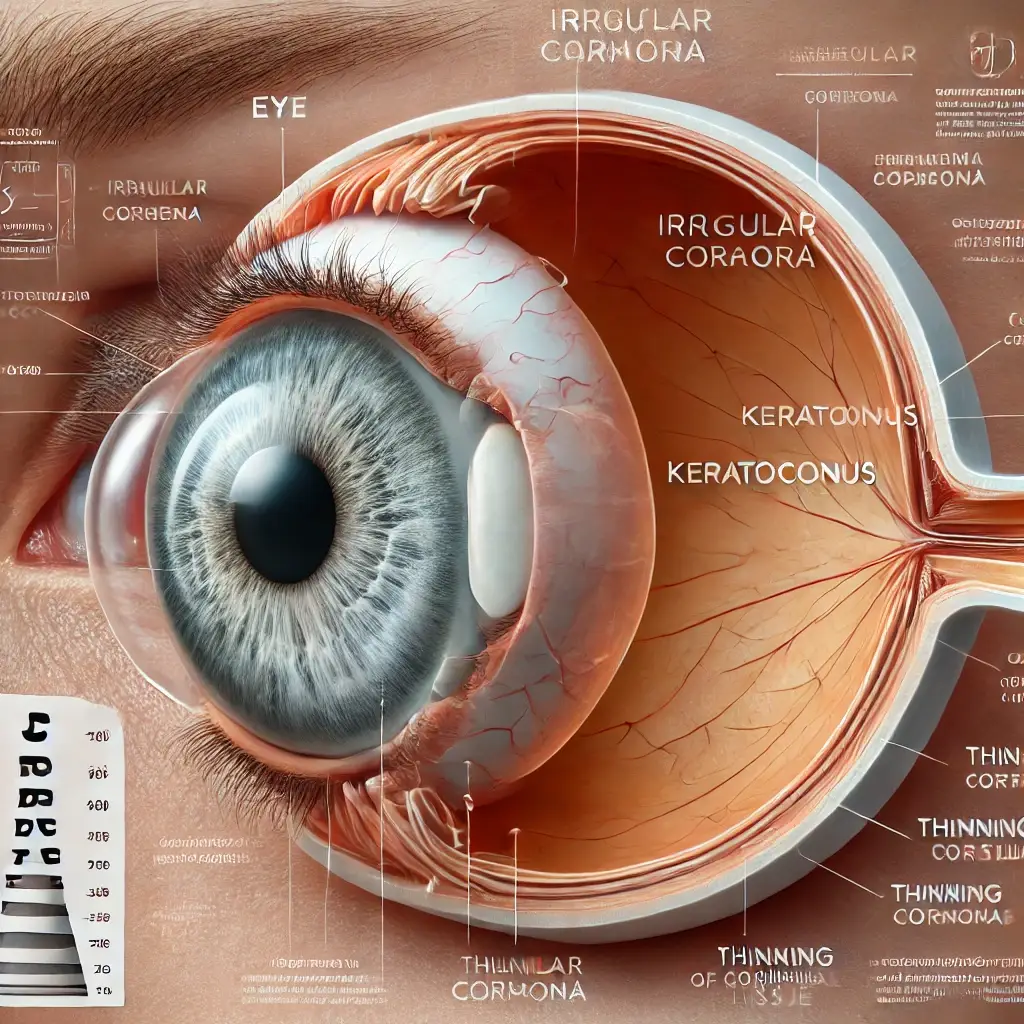
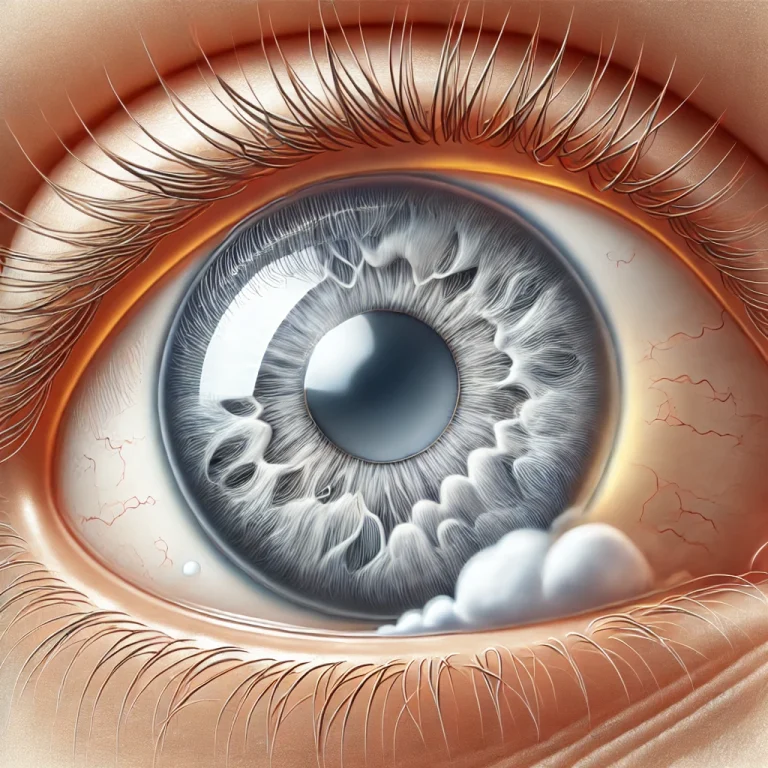
Keratoconus is a progressive eye condition that affects the shape of the cornea, causing it to thin and bulge into a cone-like shape. This distortion can lead to blurred vision, sensitivity to light, and difficulty seeing at night. While keratoconus is a challenging condition, the good news is that there are a variety of treatment options available to help manage and improve the quality of vision for those affected.
At SymptomSync, we are committed to helping you understand the full range of Keratoconus Treatments. In this post, we will explore the causes, symptoms, and various Keratoconus treatment options for this condition. Whether you’re seeking information on traditional treatments, the latest advancements, or natural remedies, we’ve got you covered.
Table of Contents
What is Keratoconus?
Keratoconus occurs when the cornea, the transparent front part of the eye, becomes weakened and starts to bulge outward into a cone shape. The cornea’s job is to focus light on the retina, and when its shape is altered, it affects the way light enters the eye. This can cause distorted and blurry vision, making it difficult to perform everyday tasks like reading, driving, and using a computer.
While the exact cause of keratoconus is not fully understood, it is thought to be related to a combination of genetic and environmental factors. The condition typically begins during adolescence or early adulthood and progresses over time, although some cases may stabilize in later years.
Symptoms of Keratoconus
The symptoms of keratoconus can vary from mild to severe, depending on the stage of the condition. Common signs include:
- Blurred or distorted vision: As the cornea changes shape, it can distort light entering the eye, leading to blurred vision.
- Frequent prescription changes: Individuals with keratoconus often experience a rapid change in their eyeglass prescription.
- Increased sensitivity to light: People with keratoconus may develop a sensitivity to glare, particularly at night.
- Difficulty seeing at night: Due to the irregular shape of the cornea, it can be harder to see in low-light conditions.
- Double vision: In advanced stages, individuals may experience double vision in one eye.
How is Keratoconus Diagnosed?
Keratoconus can be diagnosed during a routine eye exam. The key to diagnosis is detecting changes in the shape of the cornea, which can be done through a series of specialized tests:
- Slit-lamp examination: This allows the doctor to closely examine the cornea for any signs of thinning or bulging.
- Corneal topography: This test maps the shape of the cornea and helps identify any irregularities.
- Pachymetry: A measurement of corneal thickness is taken to assess the extent of thinning.
- Retinoscopy and keratometry: These tests help determine the degree of astigmatism caused by the changes in the cornea.
Keratoconus Treatment Options
While keratoconus is a progressive condition, there are many treatment options available to slow its progression, correct vision, and improve quality of life. The treatment choice will depend on the severity of the condition, the patient’s age, and their overall eye health. Let’s explore the most common treatment options for keratoconus:
1. Glasses and Contact Lenses
In the early stages of keratoconus, vision correction with eyeglasses or soft contact lenses may be sufficient. However, as the condition progresses, the irregular shape of the cornea may cause the lenses to be less effective. In these cases, more specialized contact lenses are often necessary:
- Rigid gas permeable (RGP) lenses: These lenses are designed to cover the irregular shape of the cornea and provide clearer vision.
- Scleral lenses: These are larger contact lenses that rest on the white part of the eye, creating a smooth surface for better vision correction.
- Hybrid lenses: These lenses combine the comfort of soft lenses with the clarity of RGP lenses, offering a compromise for those with keratoconus.
2. Corneal Cross-Linking (CXL)
Corneal cross-linking is a non-surgical procedure designed to strengthen the cornea and halt the progression of keratoconus. This treatment involves applying riboflavin (vitamin B2) drops to the cornea and then exposing the eye to ultraviolet (UV) light. This process creates bonds between the collagen fibers in the cornea, making it more rigid and preventing further bulging.
Corneal cross-linking is often recommended for individuals in the early to moderate stages of keratoconus and can significantly slow the progression of the condition.
3. Intacs (Intracorneal Ring Segments)
Intacs are small, curved implants that are inserted into the cornea to reshape it and improve vision. These implants are designed to flatten the cornea and reduce the bulging that causes blurred vision. Intacs are typically used in individuals with mild to moderate keratoconus who are not good candidates for corneal transplants.
This procedure is reversible, meaning that the implants can be removed or replaced if necessary.
4. Corneal Transplant Surgery
In cases of advanced keratoconus where other treatments have not been effective, a corneal transplant (also known as a penetrating keratoplasty) may be recommended. This procedure involves replacing the damaged cornea with a healthy donor cornea. While corneal transplants can significantly improve vision, the recovery process is lengthy, and the risk of complications such as infection or rejection of the donor tissue is higher.
There are two main types of corneal transplant surgery:
- Penetrating keratoplasty (PK): A full-thickness transplant of the cornea.
- Deep anterior lamellar keratoplasty (DALK): A partial-thickness transplant, preserving the inner layers of the cornea.
Treatment Comparison: A Quick Guide
Here’s a table comparing different treatment options for keratoconus:
| Treatment | Stage of Keratoconus | Procedure | Benefits | Risks |
|---|---|---|---|---|
| Glasses and Contact Lenses | Early stage | Corrective lenses or glasses | Non-invasive, easy to manage | Limited effectiveness in advanced stages |
| Corneal Cross-Linking (CXL) | Early to moderate stage | UV light treatment with riboflavin drops | Slows progression, non-surgical | Temporary discomfort, risk of infection |
| Intacs | Mild to moderate stage | Surgical insertion of curved corneal implants | Improves vision, reversible | Possible complications with implants |
| Corneal Transplant | Advanced stage | Full or partial corneal transplant | Significant vision improvement | Long recovery, risk of rejection |
Natural Remedies for Keratoconus (Supporting Treatments)
While medical treatments are essential for managing keratoconus, some individuals also turn to natural remedies to support eye health. These remedies are not substitutes for professional treatment but may help improve overall eye comfort:
- Omega-3 Fatty Acids: These healthy fats, found in fish oil, can help reduce inflammation and support general eye health.
- Vitamin C: Vitamin C is an antioxidant that helps strengthen the collagen in the cornea, which may benefit those with keratoconus.
- Antioxidant-rich foods: Eating a diet rich in antioxidants, such as fruits and vegetables, can help combat oxidative stress that may contribute to the progression of eye diseases.
FAQs (Frequently Asked Questions)
1. Can keratoconus be cured? There is no known cure for keratoconus, but various treatments can help manage the condition and improve vision. Early intervention can slow the progression, and treatments like corneal cross-linking or surgery can provide significant benefits.
2. How long does it take to recover from corneal cross-linking? Most patients experience a recovery time of around 1-3 months after corneal cross-linking. During this period, it’s essential to follow post-operative care instructions to ensure proper healing.
3. Is keratoconus hereditary? Yes, keratoconus can run in families, indicating a genetic component. If you have a family history of the condition, you may be at a higher risk.
4. Are there any lifestyle changes that can help with keratoconus? While lifestyle changes won’t cure keratoconus, maintaining a healthy diet, using eye protection, and following your eye doctor’s recommendations can help reduce symptoms and slow progression.
5. Can contact lenses help with keratoconus? Yes, specialized contact lenses like rigid gas permeable (RGP) lenses or scleral lenses can be very effective in managing keratoconus by providing clearer vision and improving the comfort of the eyes.
If you’d like more in-depth information on any of the treatments mentioned, feel free to visit SymptomSync for additional resources.

Leave a Reply