Can Cataracts Come Back? What You Need to Know
Cataract surgery is one of the most common and successful procedures performed worldwide. It restores clear vision for millions of people every year. However, a common question that many patients have is whether cataracts can come back after surgery. This question often causes confusion, as many people believe that cataracts, once removed, are permanently gone. In this blog post, we will explore the truth behind whether cataracts can return, what can affect the outcome of cataract surgery, and how you can manage your eye health to prevent future problems.
At SymptomSync, we aim to provide you with the latest and most accurate information regarding health conditions. If you’re wondering about the longevity of your cataract surgery results, read on to find out more!
Table of Contents
What are Cataracts?
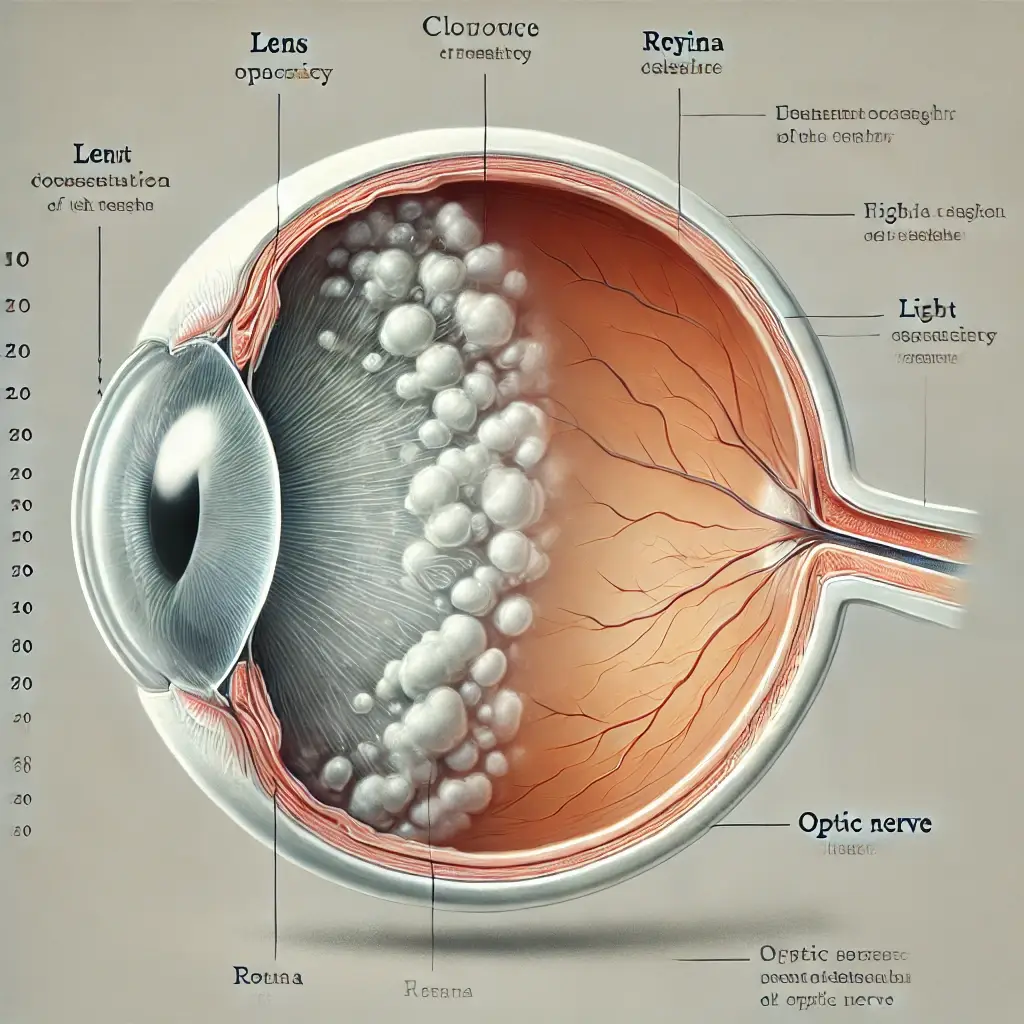
Before diving into whether cataracts can return, it’s essential to understand what cataracts are. A cataract is a condition that causes the lens of the eye to become cloudy, leading to blurry vision. Cataracts are typically age-related, though they can also be caused by other factors like injury, medication, or genetic conditions.
The only way to treat cataracts is through surgery. During cataract surgery, the clouded lens is removed and replaced with an artificial intraocular lens (IOL), which restores clear vision.
Can Cataracts Come Back After Surgery?
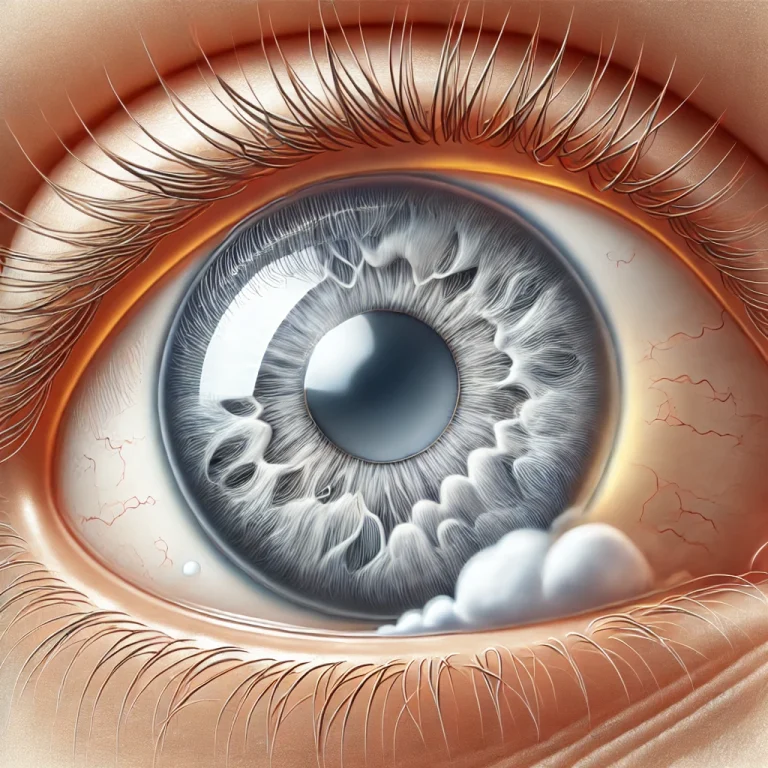
The short answer is no, cataracts cannot come back after the surgery. Once the natural lens of the eye is removed and replaced with an IOL, the cataract is gone for good. However, there’s something called posterior capsule opacification (PCO) that can cause vision problems after cataract surgery, which is often mistaken for a “return” of the cataract.
What is Posterior Capsule Opacification (PCO)?
PCO occurs when the thin membrane that holds the IOL in place (known as the posterior capsule) becomes cloudy after surgery. This clouding can cause blurry or hazy vision, similar to the symptoms of cataracts. PCO is not a cataract, but it is a common complication following cataract surgery.
PCO typically develops months or even years after cataract surgery. It can happen in 20-30% of patients who undergo cataract surgery. Fortunately, if PCO occurs, it can be treated easily with a quick, painless procedure called YAG laser capsulotomy. This procedure uses a laser to create an opening in the cloudy membrane, restoring clear vision without the need for further surgery.
If you're curious about how YAG laser capsulotomy works, you can learn more here.
Why Does PCO Happen?
PCO happens because the natural lens capsule, which is left in place during cataract surgery to support the IOL, can sometimes become cloudy over time. This cloudiness is caused by the growth of lens epithelial cells that remain after the lens is removed. These cells can migrate and proliferate on the posterior capsule, causing it to become cloudy.
While PCO is a relatively minor complication, it is essential to be aware of its possibility and consult with your ophthalmologist if you experience blurry vision or other symptoms after cataract surgery.
How to Prevent PCO?
Although PCO is not entirely preventable, several factors can reduce the likelihood of it occurring after cataract surgery:
- Choosing the Right Surgeon: A skilled and experienced surgeon can minimize the risk of PCO. Choosing a surgeon who uses advanced techniques and tools can help reduce the chances of complications.
- Using Modern IOLs: Some types of intraocular lenses are designed to help reduce the risk of PCO. For example, certain lenses have a specific coating or design that makes it more difficult for cells to grow on the posterior capsule.
- Post-Surgery Care: Following post-surgery instructions carefully, including attending follow-up appointments, can help ensure that any issues are caught early and addressed promptly.
Other Complications After Cataract Surgery
While PCO is the most common complication after cataract surgery, there are other potential issues that could affect your vision. Some of these include:
- Infection: Although rare, an infection known as endophthalmitis can occur after cataract surgery. This infection can cause pain, redness, and loss of vision. It’s important to follow your surgeon’s instructions to minimize this risk.
- Retinal Detachment: Some people may experience retinal detachment after cataract surgery, though this is also rare. Symptoms may include sudden flashes of light, floaters, or a curtain-like shadow over your vision.
- Intraocular Lens Displacement: In rare cases, the IOL can shift out of place. If this happens, additional surgery may be required to reposition the lens.
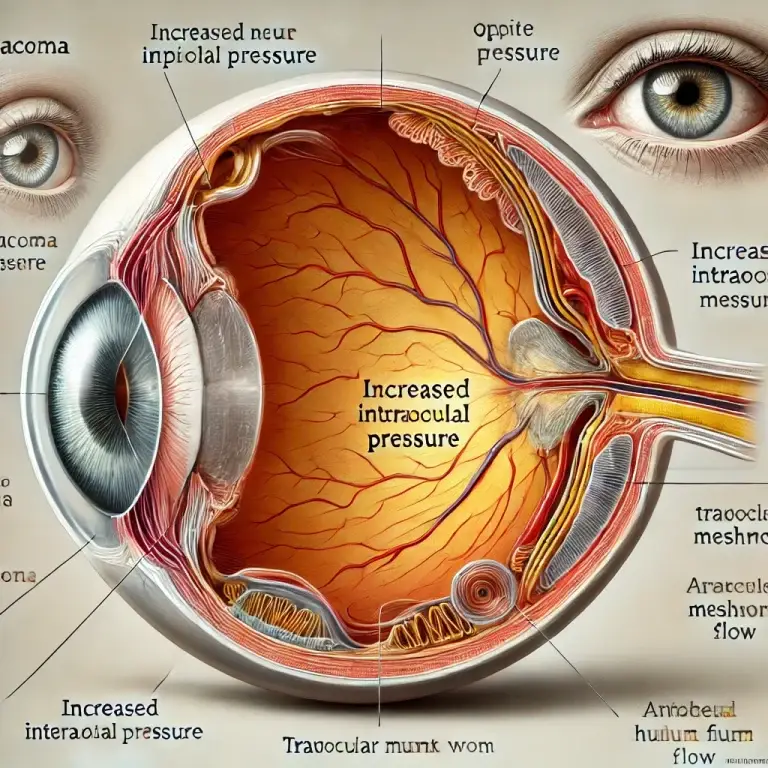
- Glaucoma: In some cases, cataract surgery can lead to an increase in eye pressure, potentially causing glaucoma. Regular eye exams after surgery will help detect this early.
When to See a Doctor After Cataract Surgery
It’s essential to attend regular follow-up appointments with your ophthalmologist after cataract surgery. However, you should also seek medical attention if you experience any of the following symptoms:
- Sudden vision loss or significant vision changes
- Pain or discomfort in the eye
- Redness or swelling around the eye
- Halos, glare, or difficulty seeing at night
These symptoms could indicate a complication that needs prompt attention.
How Long Does It Take to Recover from Cataract Surgery?
The recovery process after cataract surgery is typically quick. Most patients can return to their normal activities within a few days. However, full recovery can take several weeks. During this time, you may need to avoid certain activities such as heavy lifting, swimming, or rubbing your eyes. Your ophthalmologist will give you detailed instructions on how to care for your eyes after surgery.
Here’s a general timeline of recovery after cataract surgery:
| Timeline | Post-Surgery Activity |
|---|---|
| First 24 Hours | Rest and avoid strenuous activities. Expect blurry vision, which is normal. |
| First Week | Follow up with your ophthalmologist. You can resume most daily activities, but avoid rubbing your eyes. |
| First Month | Gradual improvement in vision. You should continue to use prescribed eye drops to prevent infection and inflammation. |
| 3-6 Months | Full recovery, though some people may continue to notice slight vision fluctuations during this period. |
Can Cataracts Come Back? Final Thoughts
While cataracts themselves cannot return after surgery, it’s important to be aware of posterior capsule opacification (PCO), which can cause symptoms similar to a cataract. Fortunately, PCO can be treated with a simple laser procedure that restores clear vision. If you experience any vision issues after cataract surgery, it’s essential to consult with your ophthalmologist to determine the cause and get the appropriate treatment.
At SymptomSync, we understand the importance of maintaining healthy vision and are dedicated to providing you with accurate and reliable health information. If you have concerns about cataracts or other eye health issues, don’t hesitate to reach out for guidance.
Frequently Asked Questions (FAQs)
1. Can I get a cataract again after surgery? No, once the natural lens is removed during cataract surgery, the cataract is permanently gone. However, posterior capsule opacification (PCO) can occur, which may need to be treated.
2. What is PCO, and how is it treated? PCO is a condition where the membrane holding the IOL becomes cloudy, causing blurry vision. It is treated with a YAG laser capsulotomy, a quick and painless procedure that restores clear vision.
3. How long does it take for PCO to develop after surgery? PCO typically develops months to years after cataract surgery. If you notice any changes in your vision, it’s important to consult your ophthalmologist.
4. Can I avoid PCO after cataract surgery? While PCO cannot be entirely prevented, the use of modern IOLs and careful post-surgery care can reduce the risk.
5. Are there other complications I should watch out for after cataract surgery? Yes, although rare, complications such as infection, retinal detachment, or IOL displacement can occur. It’s important to follow up with your ophthalmologist regularly.
Read about: Keratoconus Treatments

Leave a Reply